As a pulmonologist, I've witnessed firsthand the transformative impact of biological therapies on patients battling severe, difficult-to-treat asthma. Each success story reaffirms my belief in the power of innovation and personalized medicine to change lives.
Biologicals, such as mepolizumab, omalizumab, dupilumab, and the latest addition, the thymic stromal lymphopoietin (TSLP) blocker tezepelumab, have reshaped the landscape of asthma management. These medications target specific pathways involved in asthma's complex inflammatory process, providing tailored treatment options for patients who have not responded to traditional therapies.
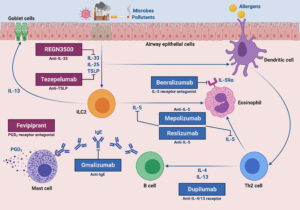
Mepolizumab, for instance, targets interleukin-5 (IL-5), a protein involved in the production of eosinophils, a type of white blood cell associated with allergic asthma. By inhibiting IL-5, mepolizumab reduces eosinophil levels, thereby decreasing airway inflammation and the frequency of asthma exacerbations.
Omalizumab works differently by targeting immunoglobulin E (IgE), an antibody involved in allergic reactions. By binding to IgE, omalizumab prevents it from triggering the allergic response, thus reducing asthma symptoms in individuals with allergic asthma.
Dupilumab is a monoclonal antibody that targets both interleukin-4 (IL-4) and interleukin-13 (IL-13), which play critical roles in the inflammatory cascade of asthma. By blocking these cytokines, dupilumab helps alleviate inflammation and improve lung function in patients with severe asthma.
The newest addition to the biological arsenal is tezepelumab, which targets TSLP, a key initiator of airway inflammation in asthma. By blocking TSLP, tezepelumab has shown promising results in reducing asthma exacerbations and improving lung function, even in patients with severe, uncontrolled asthma.
One patient who stands out in my memory is Sarah, a vibrant 35-year-old woman who had been grappling with allergic asthma for years. Despite her unwavering determination, Sarah's asthma remained stubbornly uncontrolled, casting a shadow over her daily life. Traditional treatments offered little relief, leaving her tethered to her inhaler and grappling with the fear of unpredictable asthma attacks.
Enter omalizumab, a biological therapy that targets the very root of Sarah's allergic asthma. It wasn't just about managing symptoms anymore; it was about reclaiming her life. Witnessing Sarah's journey from a life plagued by uncertainty to one filled with newfound freedom and vitality was nothing short of inspiring. Seeing her joy as she described her ability to enjoy outdoor activities without the looming fear of an asthma flare-up reminded me of why I chose this profession—to make a tangible difference in the lives of my patients.

Then there's Ahmed, a resilient 45-year-old man whose battle with severe eosinophilic asthma had taken a toll on both his physical and emotional well-being. Despite his stoic demeanor, it was evident that John was weary from the relentless cycle of exacerbations and hospital visits. Conventional therapies had failed to provide the relief he so desperately sought, leaving him trapped in a seemingly endless struggle.
Introducing mepolizumab into John's treatment regimen was a game-changer. Watching him regain control over his asthma was nothing short of miraculous. Gone were the days of constant worry and dependence on oral steroids. Instead, John found himself embracing life with a newfound sense of optimism and vitality. His laughter, once stifled by the burden of his condition, now echoed throughout the clinic, a testament to the transformative power of modern medicine.
But it's not just about the remarkable success stories; it's also about recognizing the importance of responsible and patient-centered care. As a pulmonologist, it's my responsibility to ensure that these cutting-edge treatments are used judiciously and in accordance with established guidelines. Biological therapies are not a one-size-fits-all solution, and it's crucial to carefully evaluate each patient's unique needs and circumstances before initiating treatment.
One of the most significant advantages of biological therapies is their ability to reduce the reliance on oral corticosteroids, which are associated with numerous side effects when used long term. By targeting specific inflammatory pathways, biologicals offer a more targeted approach to asthma management, reducing the need for systemic steroids and their associated adverse effects, such as weight gain, diabetes, osteoporosis, and increased susceptibility to infections.
Furthermore, biological therapies are administered via prefilled pens, making them convenient and easy to use, even for patients who may struggle with traditional inhaler devices. This user-friendly delivery system enhances treatment adherence and empowers patients to take control of their asthma management.
However, despite their remarkable efficacy, it's essential to use biological therapies judiciously and according to established guidelines. These medications are not without risks, and appropriate patient selection and monitoring are crucial to ensure their safe and effective use. Moreover, biologicals should be reserved for patients with severe, uncontrolled asthma who have failed to respond to standard therapies, as inappropriate use may lead to unnecessary healthcare costs and potential adverse effects.
In closing, the advent of biological therapies has reshaped the landscape of asthma management, offering hope and renewed optimism to patients who once felt trapped by their condition. As a pulmonologist, I am humbled and privileged to be a part of this journey, bearing witness to the transformative power of medicine and the resilience of the human spirit. Together, we can continue to breathe new life into the fight against asthma, one patient at a time.
PS Names and age changed, to protect the privacy

