Intercostal Chest Tube Drainage
 Intercostal chest tube drainage, also known as intercostal drain or chest tube insertion, is a medical procedure in which a flexible tube is placed into the pleural space (the space between the lungs and the chest wall) to drain fluid, blood, or air and restore normal lung function. It is typically performed to treat conditions such as pneumothorax (collapsed lung), hemothorax (blood in the pleural space), or pleural effusion (excess fluid in the pleural space).
Intercostal chest tube drainage, also known as intercostal drain or chest tube insertion, is a medical procedure in which a flexible tube is placed into the pleural space (the space between the lungs and the chest wall) to drain fluid, blood, or air and restore normal lung function. It is typically performed to treat conditions such as pneumothorax (collapsed lung), hemothorax (blood in the pleural space), or pleural effusion (excess fluid in the pleural space).
Here is an overview of the steps involved in intercostal chest tube drainage:
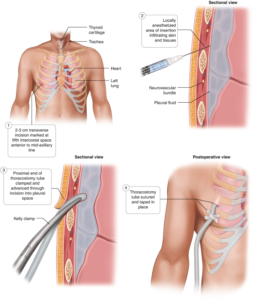
1. Preparation: The patient is positioned typically in a semi-reclining or lateral decubitus position. The skin over the insertion site is cleaned and sterilized, and the area is numbed with a local anesthetic to minimize discomfort.
2. Incision and tube insertion: A small incision is made in the skin, usually between the ribs, in the appropriate intercostal space based on the condition being treated. A blunt dissection technique is used to create a pathway through the muscles and tissues to reach the pleural space. A trocar or a dilator may be used to assist in creating the tract.
3. Chest tube placement: A flexible plastic or rubber tube, known as a chest tube or thoracic catheter, is inserted through the incision and advanced into the pleural space. The tube is typically secured to the skin using sutures or adhesive dressings to prevent movement or dislodgement.
4. Drainage and suction: The other end of the chest tube is connected to a drainage system, which can be a closed drainage system or a water seal system. The drainage system allows the fluid, blood, or air to be evacuated from the pleural space. In some cases, suction may be applied to the drainage system to enhance the removal of fluid or air.
5. Monitoring and observation: The patient's vital signs, lung sounds, and drainage output are closely monitored following chest tube insertion. X-rays or other imaging modalities may be performed to confirm the proper placement of the tube and assess lung re-expansion.
6. Duration and removal: The chest tube is typically left in place until the drainage resolves or diminishes significantly, and the lung has re-expanded. This duration can vary depending on the underlying condition and the patient's response to treatment. Once the drainage has decreased, the chest tube is carefully removed, and the incision is dressed and monitored for any signs of complications.
Intercostal chest tube drainage is a common procedure performed by trained healthcare professionals, such as surgeons, interventional radiologists, or pulmonologists. It aims to alleviate symptoms, promote lung re-expansion, and facilitate the resolution of conditions affecting the pleural space. The procedure requires careful monitoring and management to minimize the risk of complications, such as infection, bleeding, or lung injury.
6. Monitoring and observation: Throughout the procedure, the patient's vital signs and oxygen levels are monitored. The healthcare provider also observes for any signs of complications, such as bleeding, infection, or lung injury.
7. Post-procedure care: After the thoracocentesis, the needle is removed, and pressure is applied to the site to prevent bleeding. A bandage is applied to cover the insertion site. The patient may be advised to take it easy and avoid strenuous activities for a short period following the procedure.
Ultrasound-guided thoracocentesis offers several advantages over traditional blind thoracentesis, such as improved accuracy and safety by visualizing the needle insertion site, minimizing the risk of complications. It allows for more precise targeting of the fluid or air collection, reducing the likelihood of injury to surrounding structures. Overall, ultrasound guidance enhances the success and safety of the thoracocentesis procedure.

